Why Atrial Fibrillation Matters

Figure 1: Atrial Fibrillation Statistics. Atrial fibrillation is a common preventable cause of stroke, yet it can be very difficult to detect.
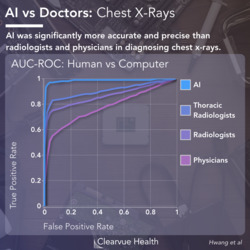
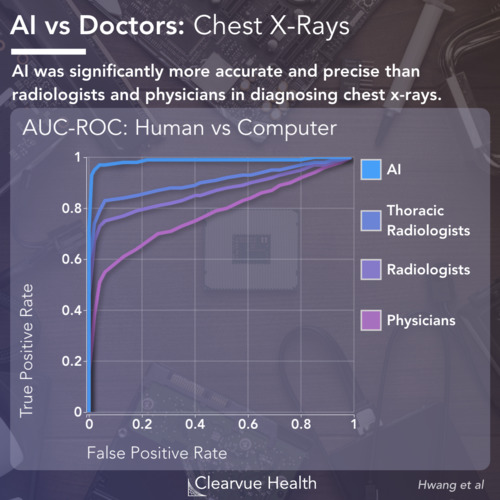
Many studies have shown significant achievements in artificial intelligence diagnosis in medicine. AI has been shown to be as good or better than humans in multiple tasks including reading x-rays and other medical images.
A new study finds that AI can detect atrial fibrillation in normal sinus rhythm, a task that is just about impossible for most human doctors.
In this article, we will review some of the context of this achievement and show why this is such a monumental breakthrough.
Source: An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction
Diagnosing Atrial Fibrillation with ECGs

Figure 2: Atrial Fibrillation vs Normal Sinus Rhythm on Electrocardiogram. During atrial fibrillation, the heart fails to beat regularly and shows an irregular rhythm on ECGs.
Atrial fibrillation has been estimated to cause around 15% of all strokes. This is concerning as much of this is preventable with good treatment. However, many patients don’t know that they have atrial fibrillation until it is too late.
Atrial fibrillation is easy to diagnose when a patient has an active episode. An electrocardiogram will show the heart failing to beat regularly. However, most patients with atrial fibrillation only occasionally experience episodes. Unless the patient is fortunate enough to be undergoing an active episode during a doctors visit, they likely will go undiagnosed.
We Miss a Lot of Cases of Atrial Fibrillation

Figure 3: Atrial Fibrillation Diagnosis Statistics. A study in Sweden estimated that out of 1000 elderly patients, around 93 will have a diagnosis of Atrial Fibrillation. Around 5 can be diagnosed with one screening visit. 25 will go undiagnosed. This study was performed among 75-76 year olds in two Swedish regions. 7173 volunteers were studied with multiple electrocardiogram tests over 2 weeks.
One study in Sweden found that out of 1000 elderly patients, about 90 will be diagnosed with atrial fibrillation. Five can be diagnosed in one screening visit. 25 will go undiagnosed, even with one screening visit.
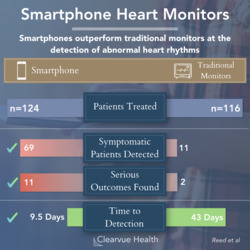
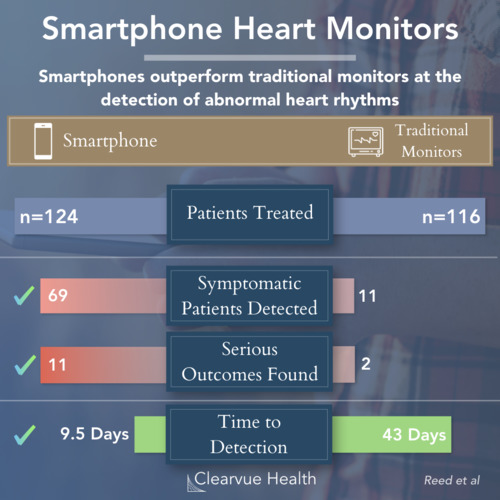
In the past, doctors have literally strapped patients with heart monitors to try to catch atrial fibrillation when it happens at home. Some smartphones have made some progress in helping with this challenge as well.
Source: Mass Screening for Untreated Atrial Fibrillation: The STROKESTOP Study.
Detection of Atrial Fibrillation in Normal Sinus Rhythm

Figure 4: Detection of Atrial Fibrillation in Normal Sinus Rhythm. An AI was able to diagnose Atrial Fibrillation during normal rhythm using signs invisible to the human eye.
This new study found that they could detect atrial fibrillation in a patient even when they are not having an active episode. This is a diagnostic feat that is typically not attempted by doctors.
By using clues invisible to the human eye, this AI was able to accomplish what was previously impossible, with reasonable sensitivity and specificity.
Source: An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction
AI Performance in Electrocardiogram Diagnosis of Atrial Fibrillation

Figure 5: AI Performance in Electrocardiogram Diagnosis of Atrial Fibrillation. Long term monitoring may provide slightly better results. However, 1 ECG was almost as good as multiple over one month.
This study has two key implications for medicine. First, it provides an entirely new way to screen for atrial fibrillation. This could potentially save many lives from stroke.
Additionally, it shows that artificial intelligence may be able to accomplish tasks that most cannot even attempt in medicine. A few studies have shown that artificial intelligence may be slightly better than humans in some tasks. This is one of the first to show that AI can be effective in a task that humans normally don’t do it all because of the difficulty.
Of course, there are a few shortcomings with the study. A sensitivity and specificity of around 80% is good, but not great. It will detect many cases, but it will also miss a few. It will result in a few false positives as well.
At the moment, this method can only be used as a screening tool in combination with other more established tools.
However, with time, it is possible that this technology will improve enough that it can be applied to everyday medical practice.