Carbs and Depression: impact of diet on common mood disorders
Low-carb diets are very popular for a variety of reasons. The diet reduces the intake of unhealthy carbs found in sugar and processed foods like white bread, pasta, and sodas. People with conditions like obesity and diabetes eat a low-carb diet to help control metrics like blood sugar and cholesterol. A low-carb diet is also favored by those looking to lose weight or maintain healthy body weight. These are the physical benefits of a low-carb diet, but what about the psychological benefits? A collection of studies have come out that support an association between carbs and mood disorders, like depression.
Carbs from sugar
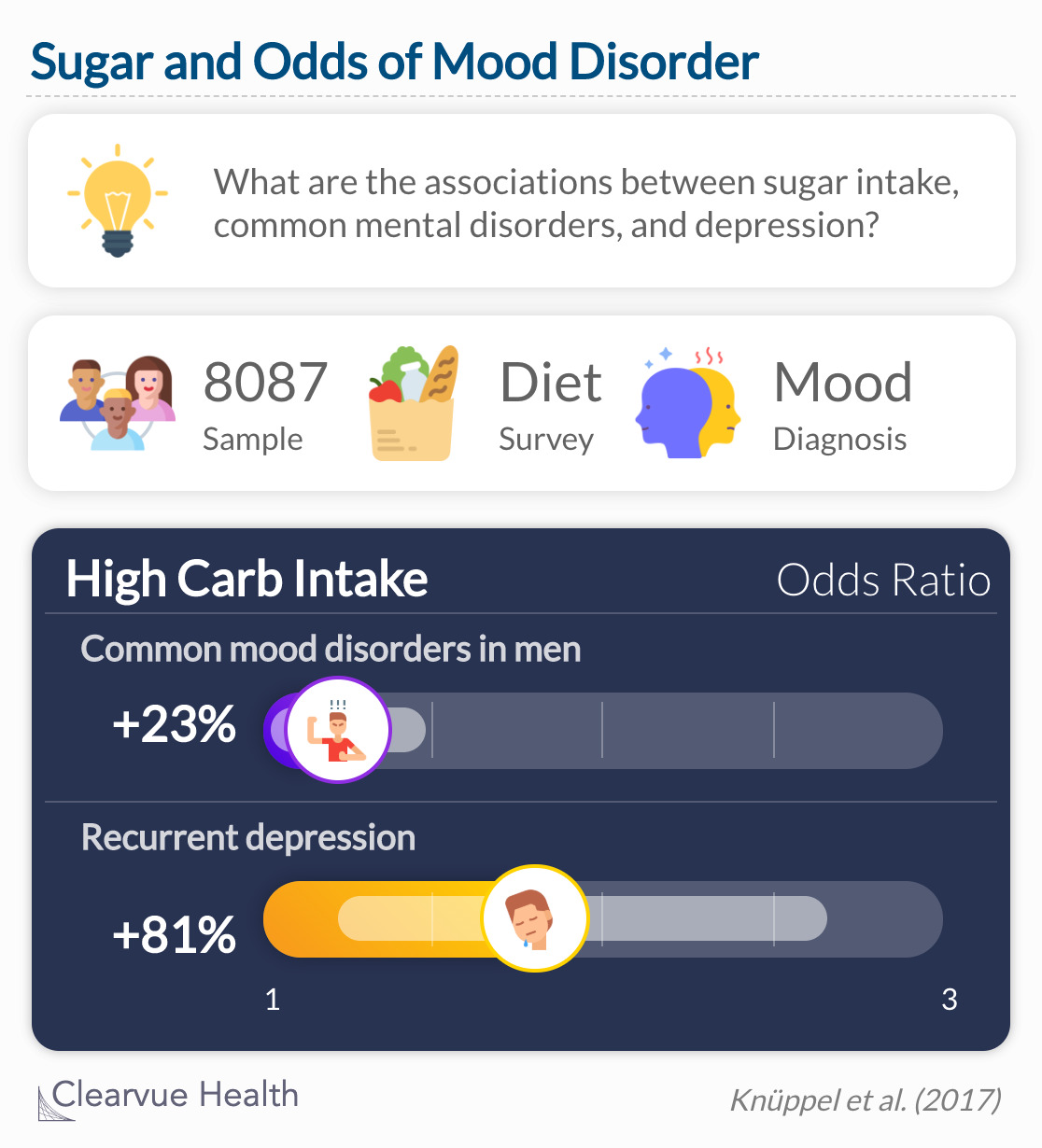
A study in Nature looked specifically at sugar as a means of carb intake. Examples of food with sugar as the main source of carbs include soda, candy, and sugary cereal. They predicted that carbs from sugar would be positively associated with the risk of depression and other mood disorders. Using data from the Whitehall II study, they compiled a sample of 8087 men and women. Diet and mood were assessed with standardized surveys administered over several years.
Men who ate 67 grams of sugar or more per day had 23% high odds of depression after five years. Men who ate 40 grams of sugar or less had a lower risk of depression.
Source: Sugar intake from sweet food and beverages, common mental disorder and depression: prospective findings from the Whitehall II study
Results showed that men who reported a high intake of sugar had the greatest odds of developing depression over the next 5 years. The results were not the same for women, who saw a less severe effect of sugar intake.
Carbs from processed foods
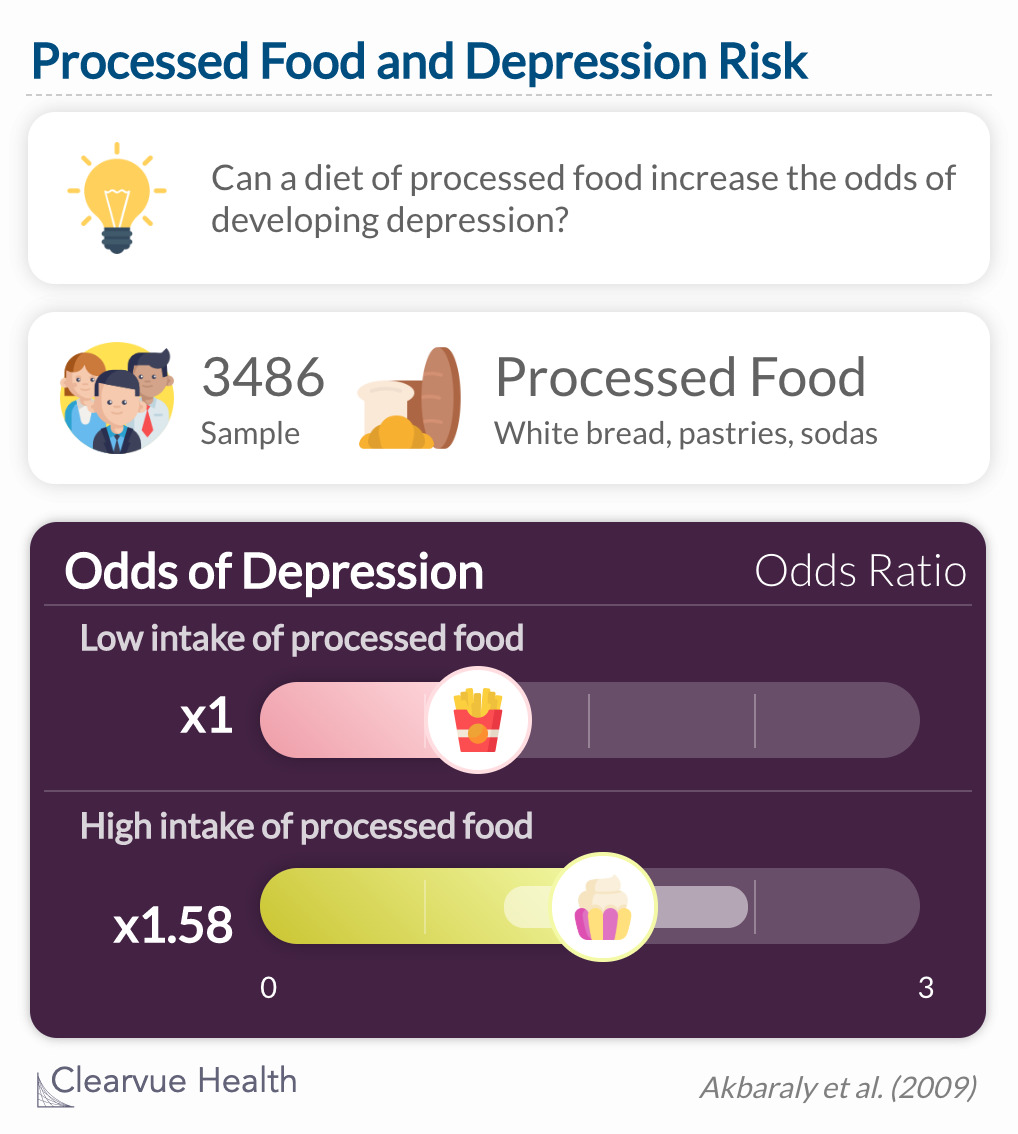
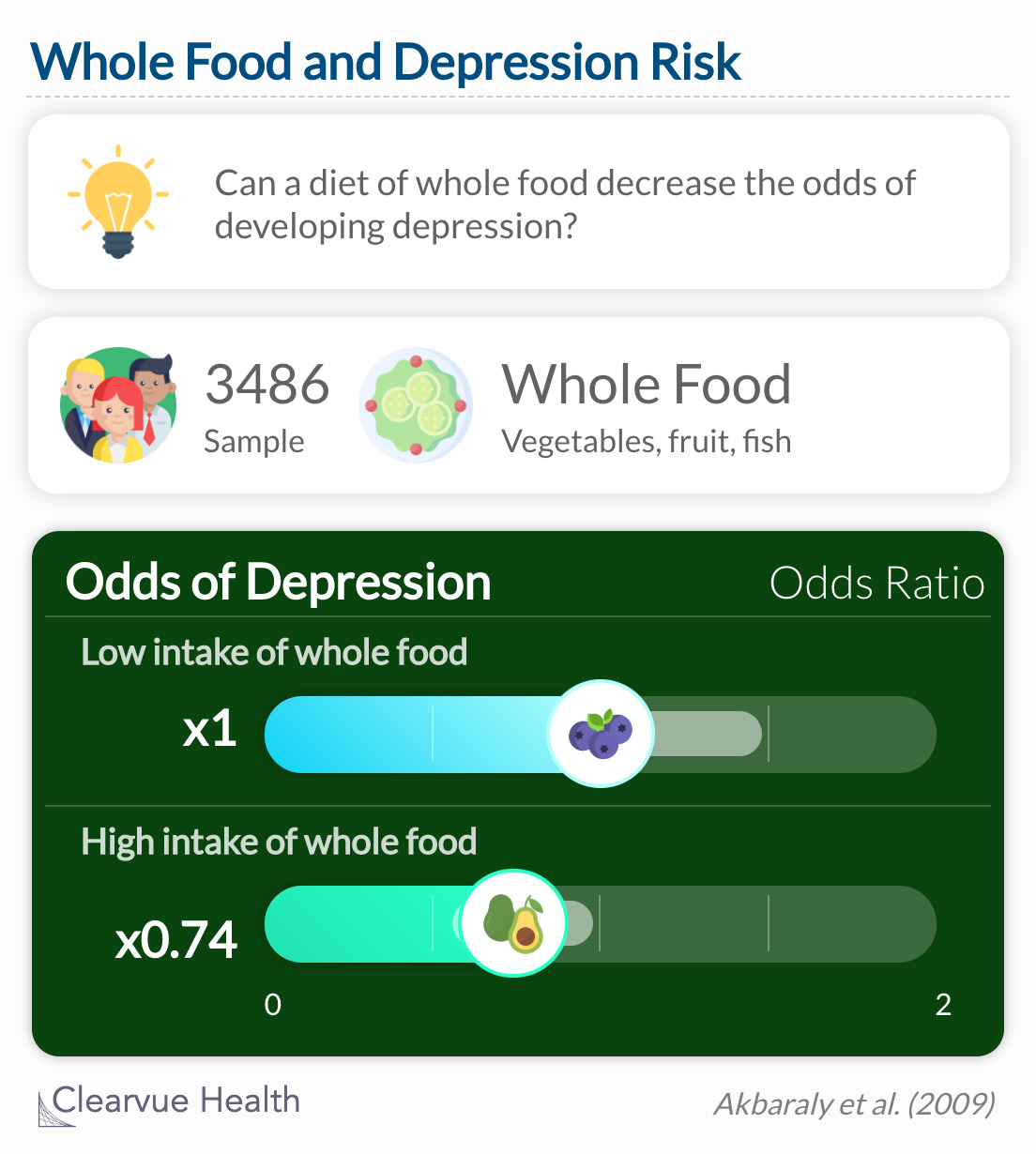
Similar results were found in a study of processed food intake and depression. Carbs are found in processed foods like white bread, pizza dough, and bakery items. Researchers gathered data on 3486 participants from the same pool as the previous sample, the Whitehall II study. In this sample, researchers split participants into two groups of dietary patterns: whole food and processed food. Whole food refers to a diet loaded with vegetables, fruits, and fish. Processed foods are high in carbohydrates as well as saturated and trans fats.
High consumption of processed food was associated with an increased odds of CES–D depression (OR = 1.58, 95% CI 1.11–2.23).
Source: Dietary pattern and depressive symptoms in middle age
Participants who abided by a whole food diet had the lowest odds of depression. As predicted, participants with the highest consumption of processed food had the greatest odds of depression.
Participants in the highest tertile of the whole food pattern had lower odds of CES–D depression (OR = 0.74, 95% CI 0.56–0.99) than those in the lowest tertile.
There are a few issues with this study that we must address. First, the entire sample was White European. The researchers excluded Black and Asian participants because they assumed their diets were too different from each other. This decision limited the generalizability of the results to White Europeans only. The results would most likely have been different if they had included a more diverse sample. Another issue is that researchers lumped all processed foods together. By doing so, they disallowed us to separate food products. In other words, we do not know for sure if the odds of depression are impacted more by carbohydrates or other components of processed food.
What came first: the carb or the depression?
There is some speculation about the direction of this relationship. Do carbs increase depression risk, or does depression increase carb intake? These studies helped answer this question. In the first study, they found a significant risk of depression after 5 years in participants who reported high carb intake. In a reverse analysis, they did not find the same effect. This supports the theory that carb intake came first, and undermined the theory that depression makes people eat more carbs.