We’ve learned over the past few months that patients with coronavirus can present different symptoms and outcomes. Some patients have a fever and a cough, while others experience neurological symptoms like a loss of smell and taste. A small percentage of patients require critical care, while others are asymptomatic and avoid the hospital completely.
To help infected patients, it is important to understand and be able to predict their related symptoms and potential complications. In this article, we examine coronavirus symptoms involving the digestive system, particularly the liver.
Data Collection
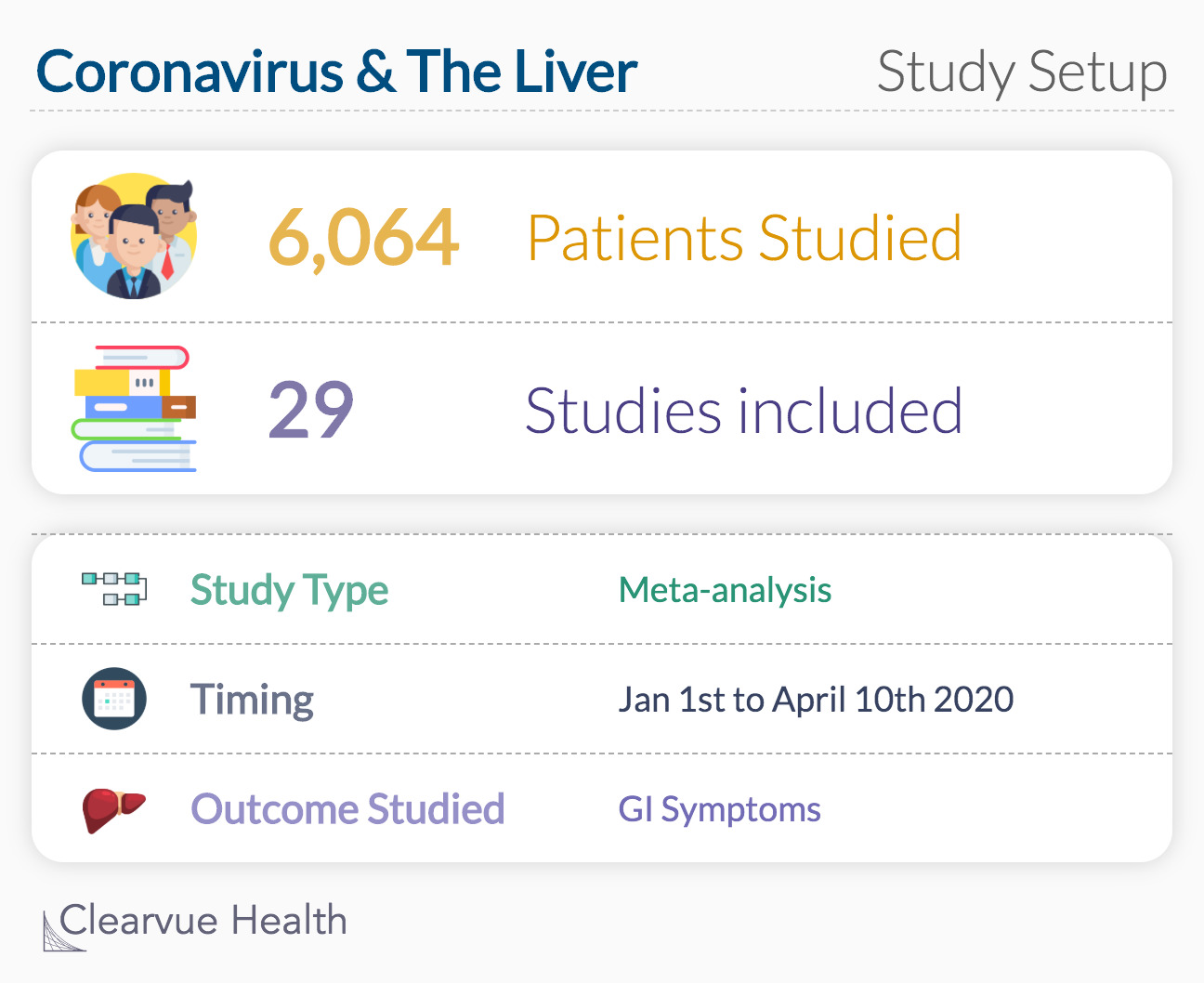
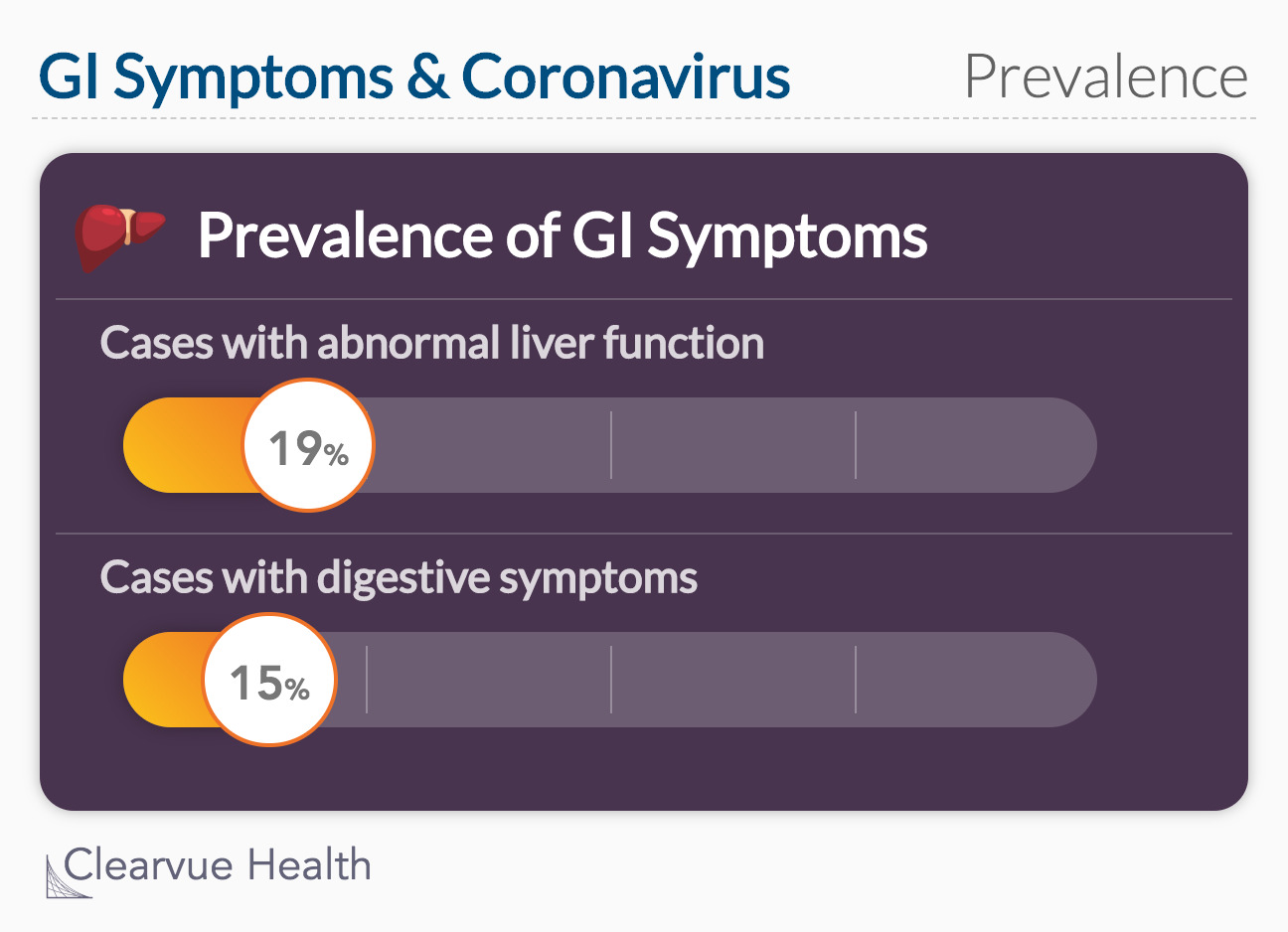
In mid-May, the Lancet published an analysis of 29 studies that reported digestive symptoms in patients with confirmed cases of coronavirus. More than six thousand patients were included in this analysis, describing symptoms such as livery injury, diarrhea, nausea, vomiting, abdominal pain, and loss of appetite.
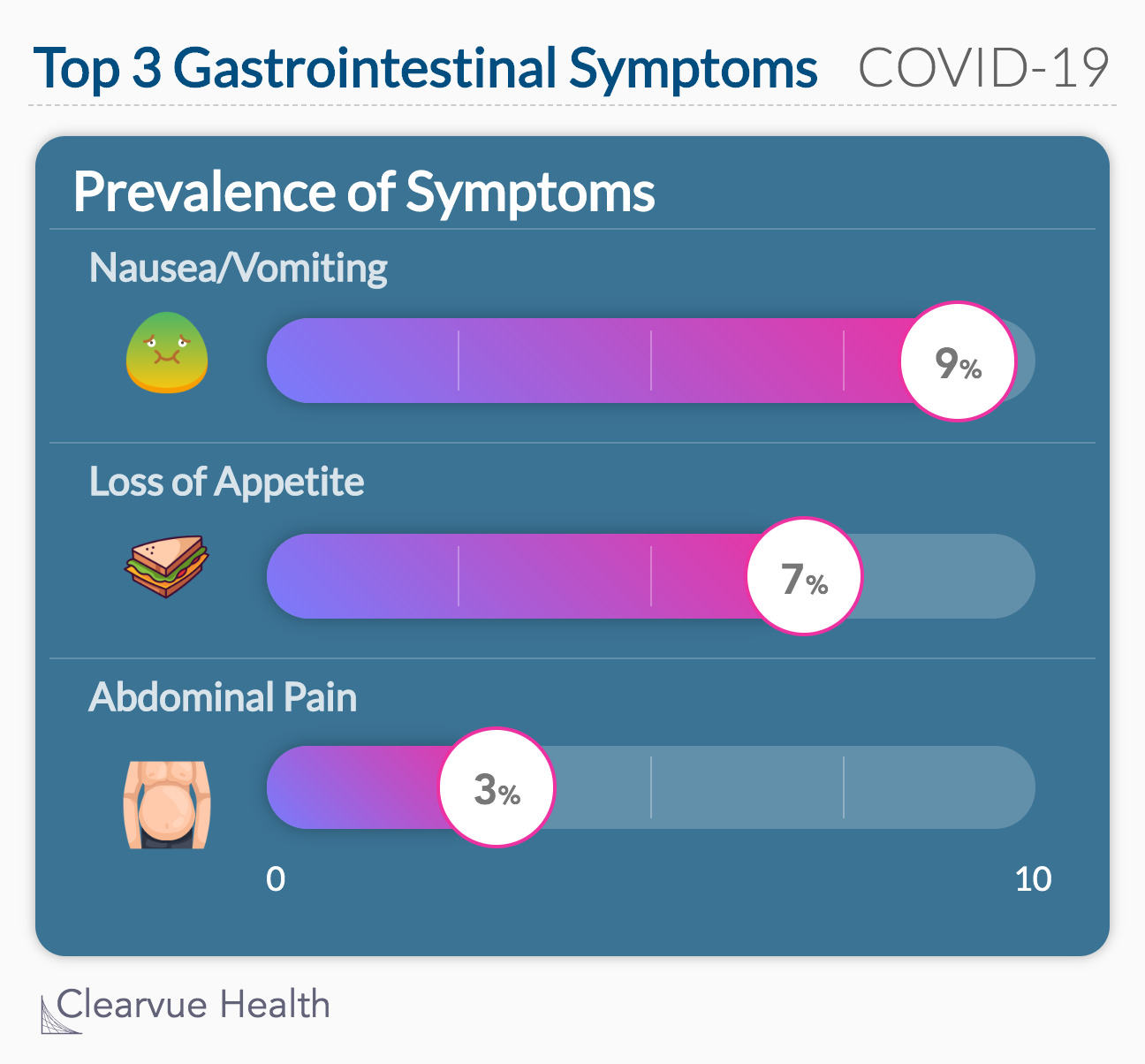
Among the studies analyzed, 12 studies with 1267 total patients reported abnormal liver function, which is about 19% of cases. An estimated 15% of confirmed coronavirus cases recorded digestive symptoms. Nausea or vomiting, diarrhea, and loss of appetite were the most common digestive symptoms.
Source: Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis
Disease severity
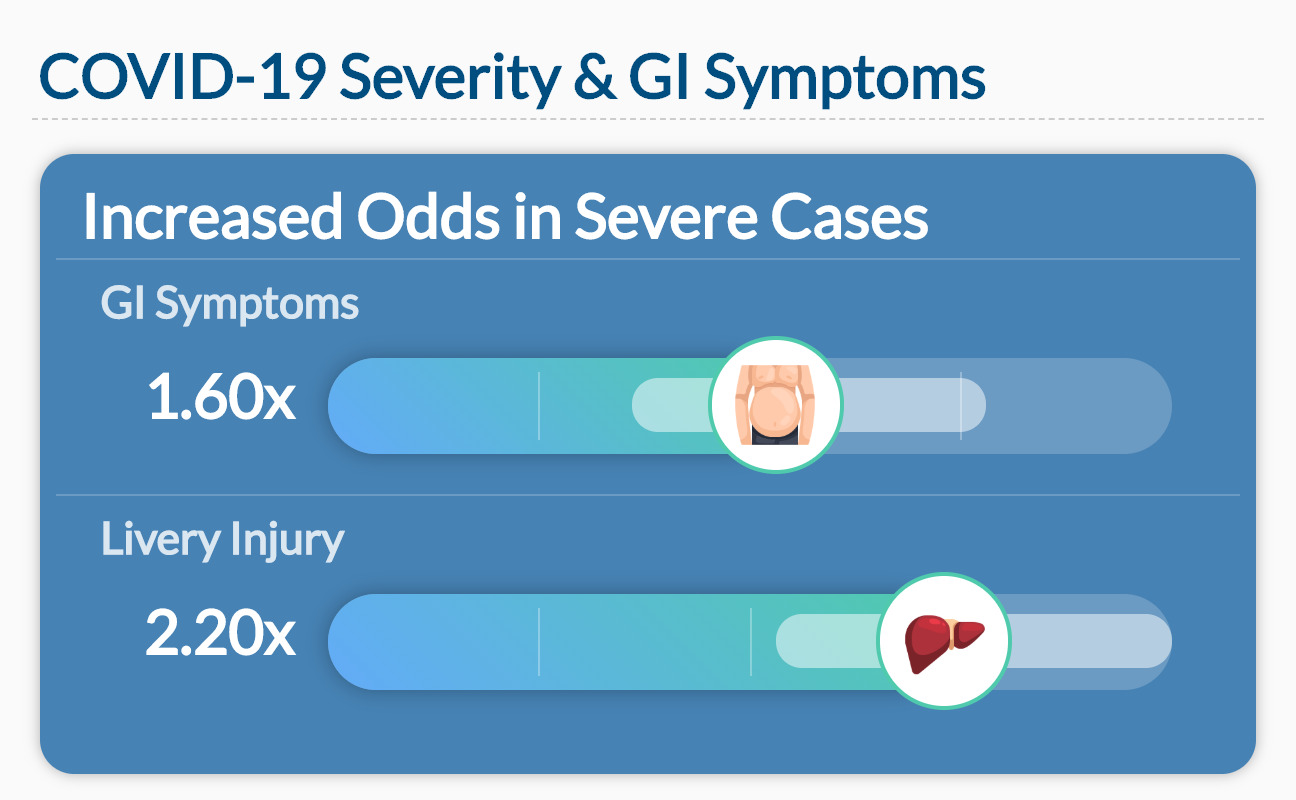
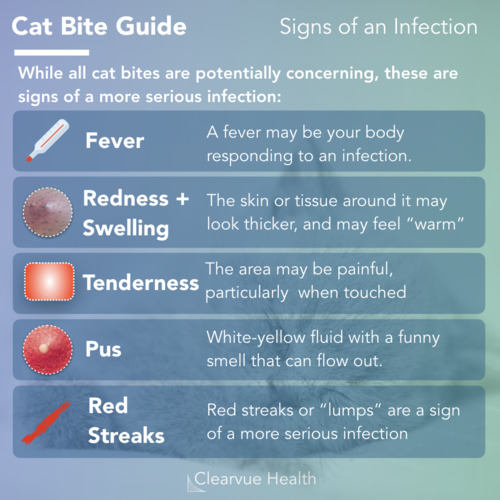
The analysis found that patients with severe cases of coronavirus had greater odds of gastrointestinal symptoms. In other words, gastrointestinal symptoms are much rarer in mild cases of coronavirus. Severe cases also showed increased odds of liver injury.
How does this happen
The liver can be harmed by inflammation or damaged cells. Scientists have a couple of theories about how the virus reaches this point. First, they considered medications. Certain medications, taken frequently, are known to damage the liver.
“
“… antibiotics, antivirals, and steroids are widely used for the treatment of COVID‐19. These drugs are all potential causes of liver injury during COVID‐19, but not yet being evident.”
Xu et al.
Source: Liver Injury During Highly Pathogenic Human Coronavirus Infections
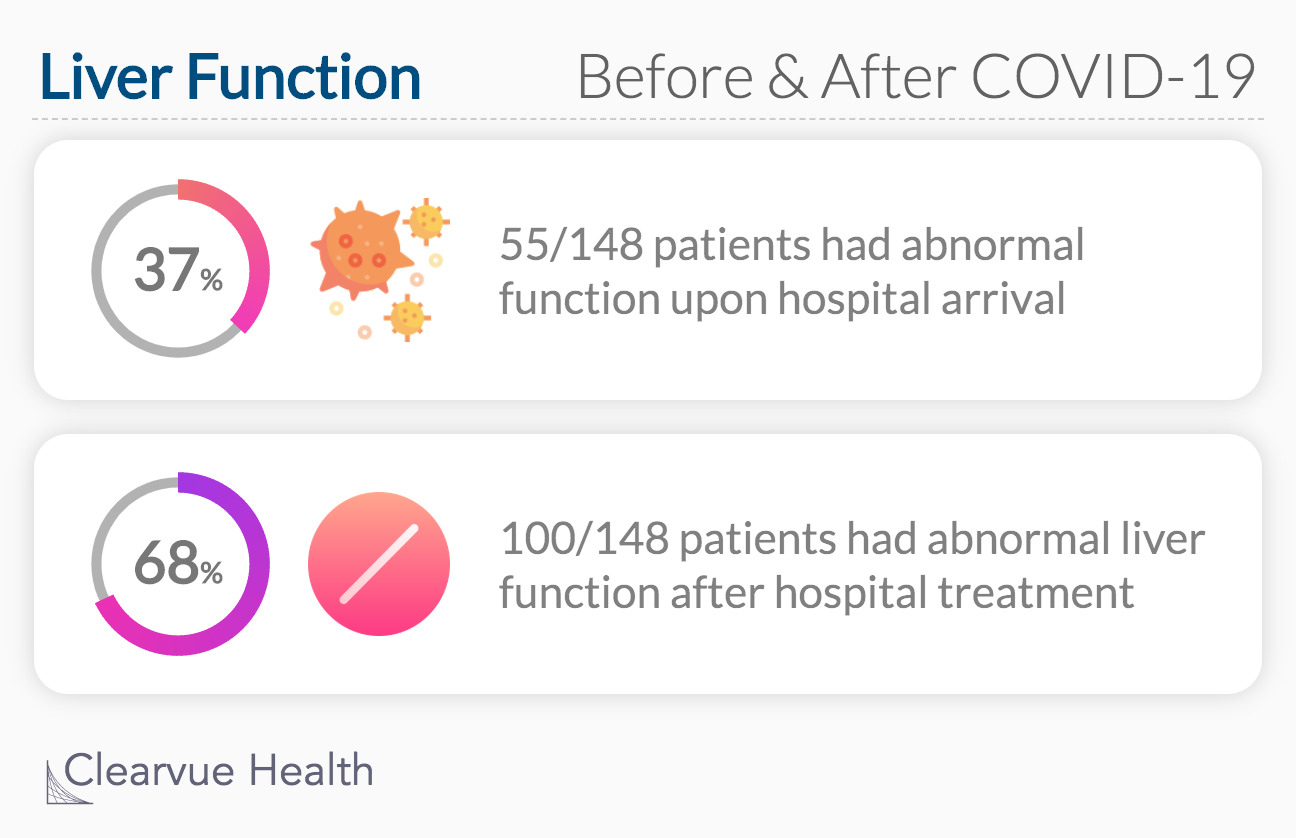
Researchers in Shanghai examined 148 coronavirus patients between January 20 - 31, 2020. Upon admission, 55 patients had an abnormal liver function and 93 patients had a normal liver function. Within 11 days after admission, 45 additional patients developed abnormal liver function.
Clinical Features of COVID-19-Related Liver Damage
To discover the root of this problem, scientists looked at the medications patients took before and during their hospital stay. Initially, they found no significant difference between groups of medication taken before hospitalization.
A review of hospital medications revealed that more patients with abnormal liver function were treated with Lopinavir/ritonavir (an antiviral drug) compared to patients with normal liver function. Doctors discourage the use of Lopinavir/ritonavir to treat coronavirus based on this potential side effect as well as the shaky evidence for its effectiveness.
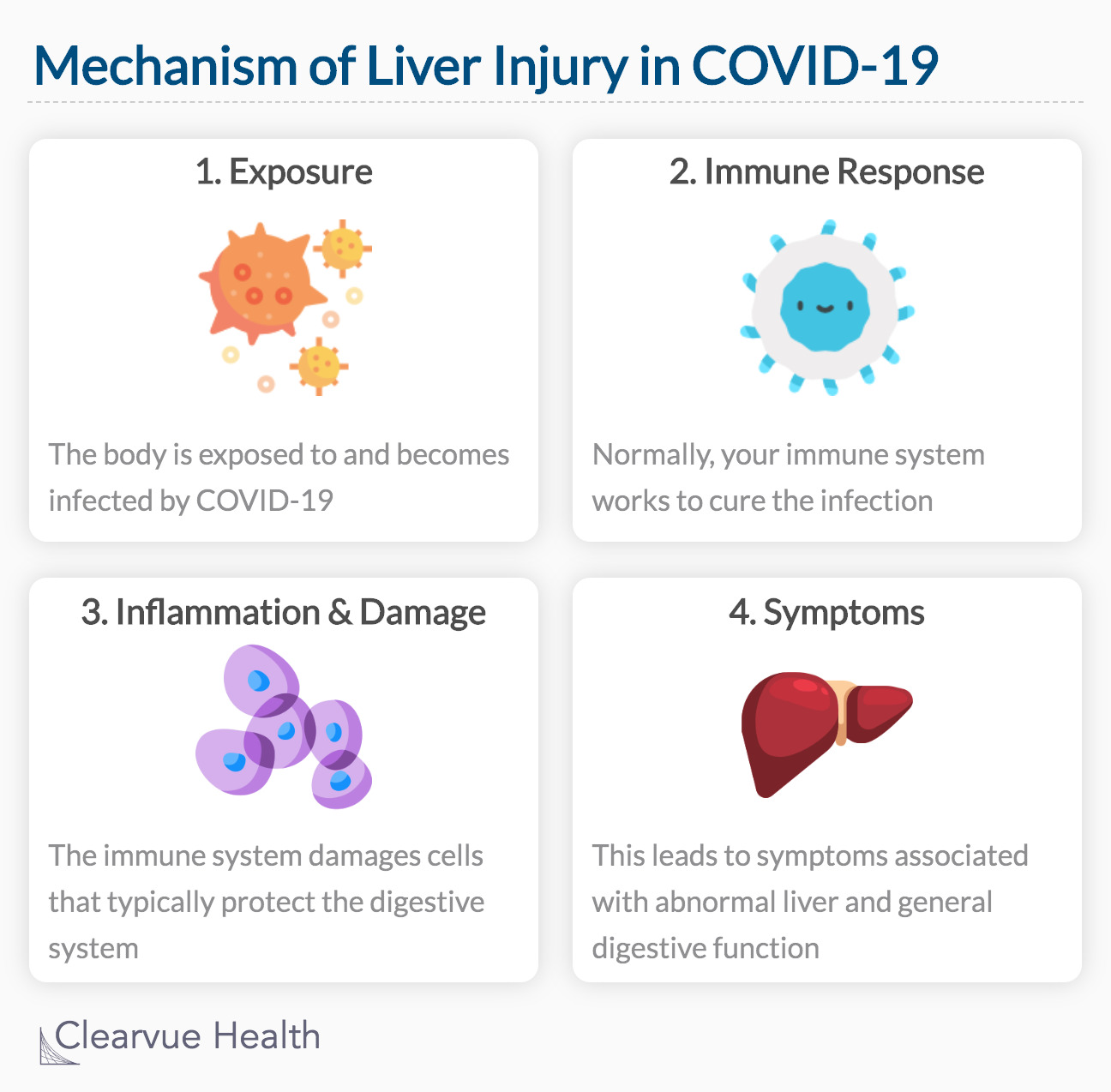
Another theory for how coronavirus may be associated with liver problems is the body’s immune response. When exposed to a virus, our immune system tries to cure the infection. Sometimes, this process can lead to inflammation or damage to specific cells. The exact path of the immune response is yet to be investigated.
Source: Liver Injury During Highly Pathogenic Human Coronavirus Infections