covid-19 and cancer: A reduction in secondary prevention practices
There is no evidence to suggest that Covid-19 causes cancer or speeds up the spread of cancer cells in the body. However, the pandemic has impacted cancer cases and deaths by reducing prevention. There are three types of prevention: primary, secondary, and tertiary. In this case, the data focus on secondary prevention, which includes tests and screenings to identify disease in its earliest stages.
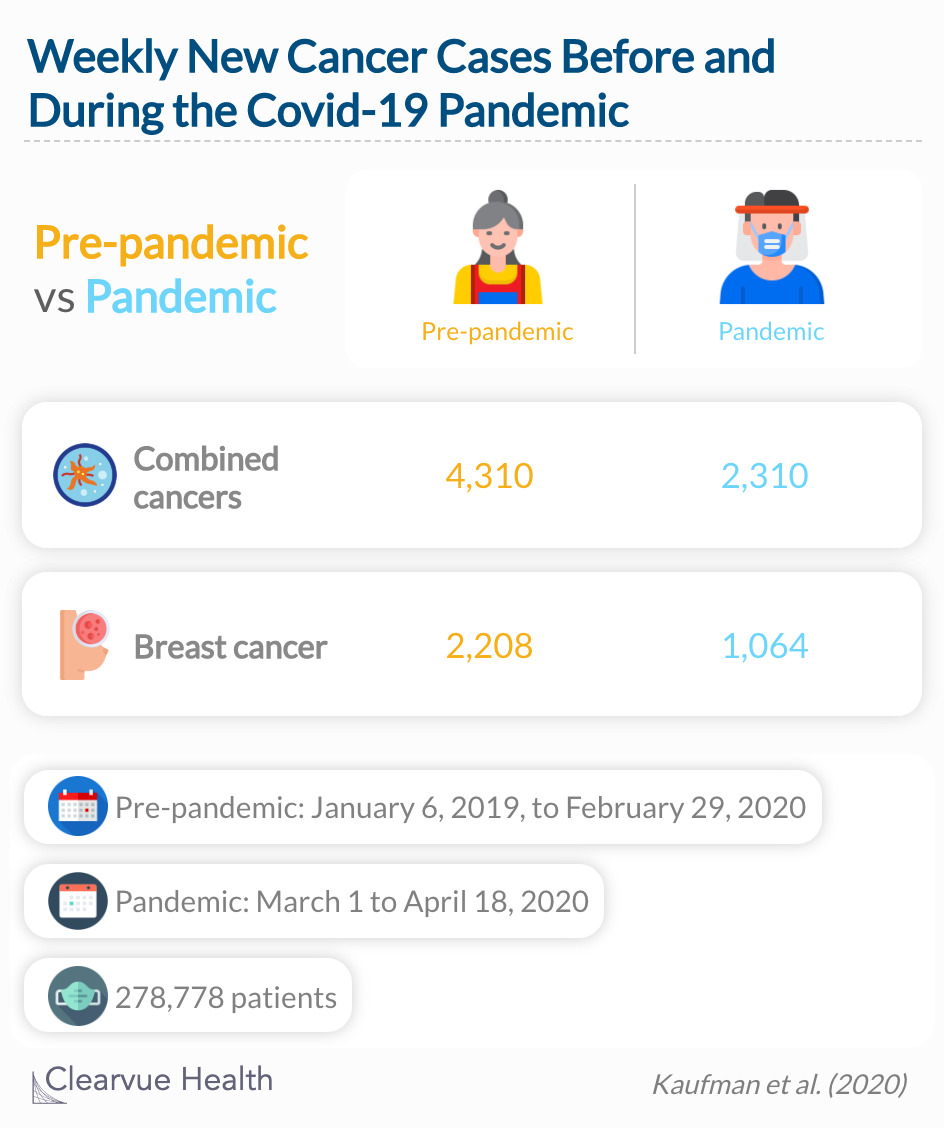
Cancer diagnoses in the US
Researchers used data from a company called Quest Diagnostics, who accept samples from doctors to confirm a cancer diagnosis. They looked at six of the most common cancers tested by the company: breast, colorectal, lung, pancreatic, gastric, and esophageal. The main goal was to compare the rates of newly diagnosed patients before and during the Covid-19 pandemic to identify any differences in testing volume. In total, 278,778 patients were included in the study.
During the pandemic, the weekly number fell 46.4% (from 4310 to 2310) for the 6 cancers combined, with significant declines in all cancer types, and similar results for colorectal cancer.
Source: Changes in the Number of US Patients With Newly Identified Cancer Before and During the Coronavirus Disease 2019 (COVID-19) Pandemic
Overall, there was a 46% decrease in the number of weekly patients diagnosed with cancer. The most significant decrease was in breast cancer diagnoses, which saw a 52% reduction in new cases. Other countries have found similar declines in cancer diagnoses and are exploring potential repercussions.
It is important to mention that this study does not list the types of testing that Quest Diagnostic performs or that is reported to them. For example, do they know about pathology results for each of these diseases? Thus, this could represent under-reporting or a skewed sample of patients whose results are handled by Quest, specifically insured patients.
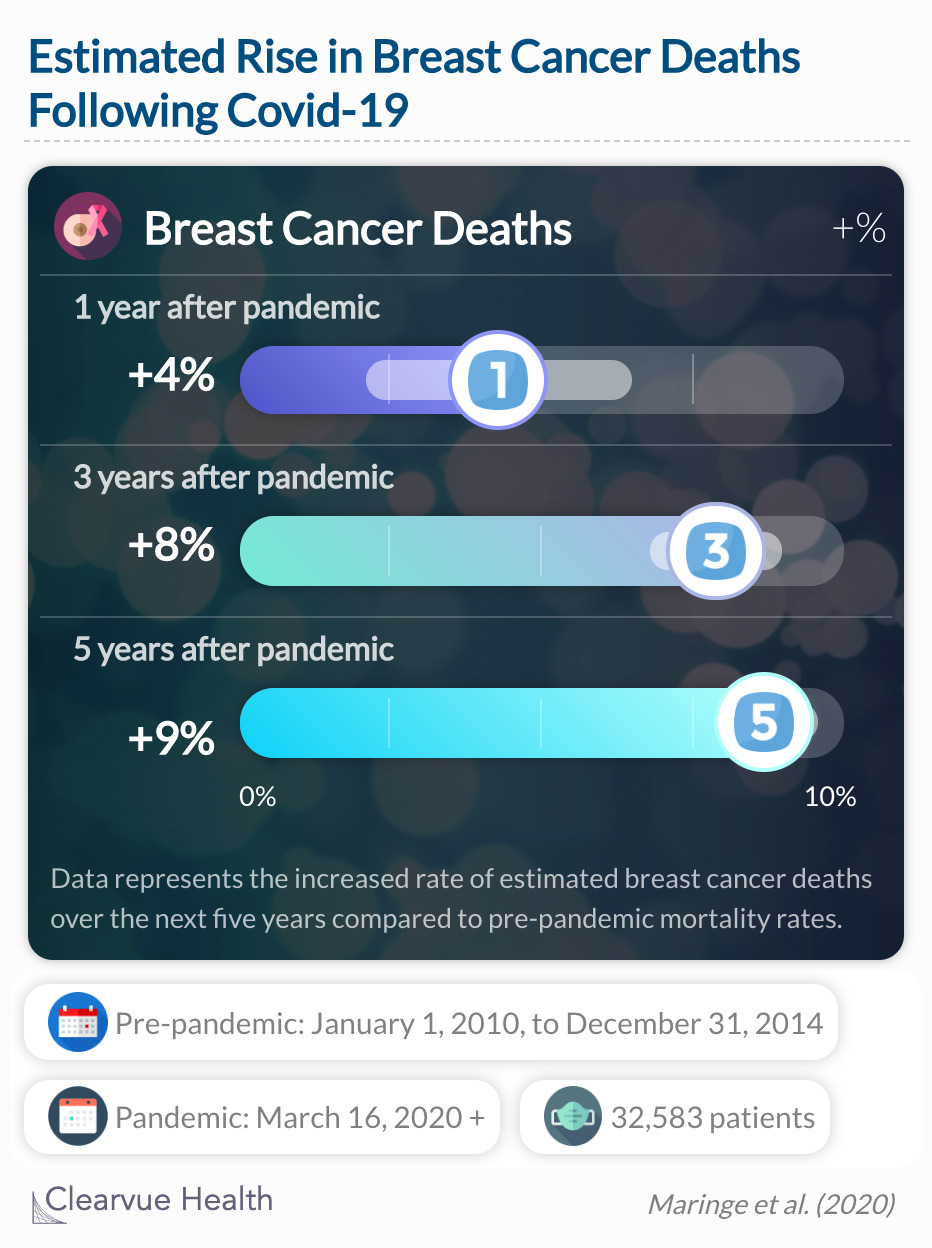
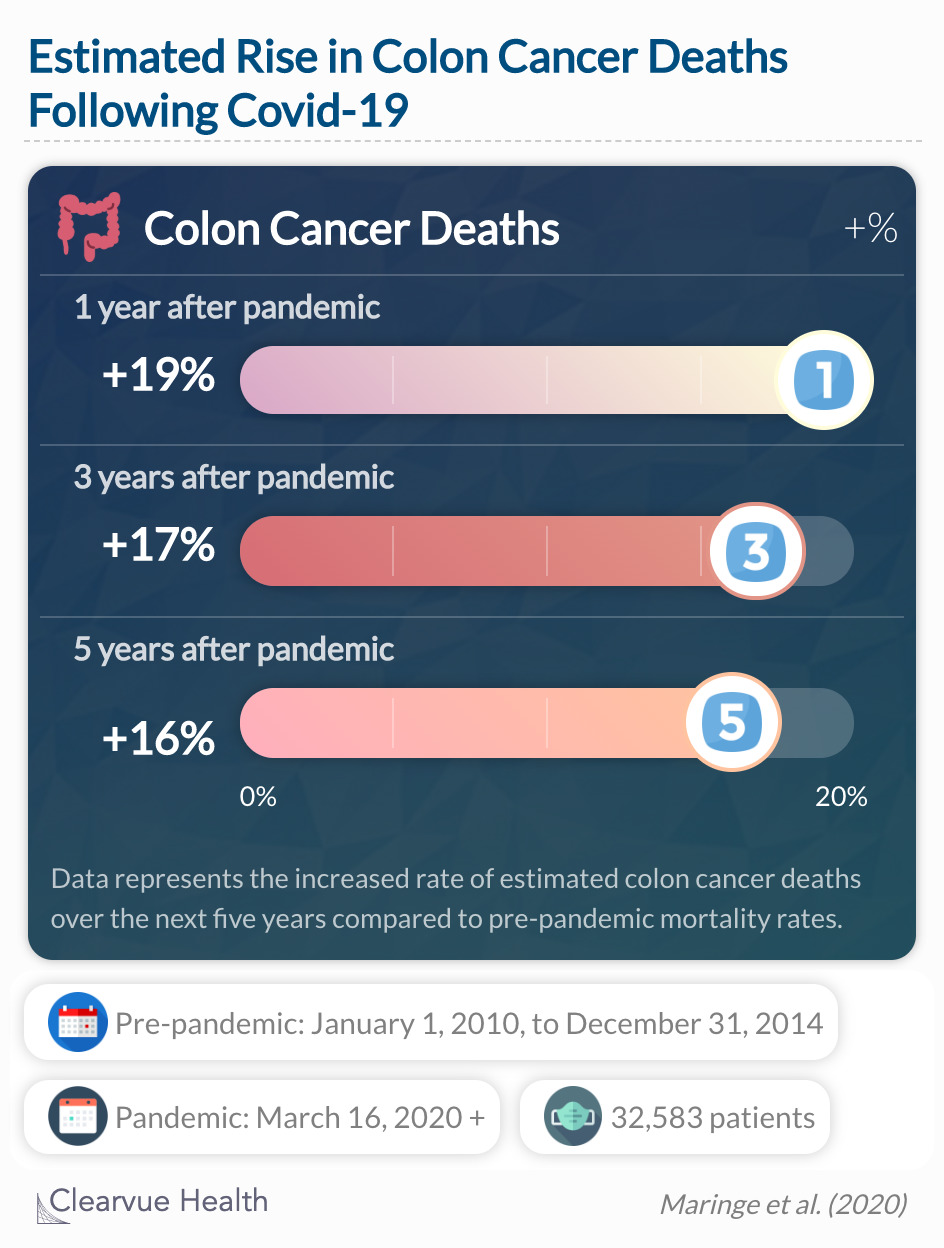
Cancer deaths in the UK
The UK recently published statistics on the impact of delays in the diagnosis of cancer survival outcomes in four cancer types during the pandemic. In this study, their pre-pandemic timeline was between 2010 through 2014. They identified deaths linked to colon, rectum, esophagus, and breast cancer from their national cancer registry and hospital databases. They estimated the impact of delayed diagnoses over the next few years.
We estimated across scenarios A–C, compared with the pre-pandemic period, a 2·1–6·6% increase in the number of deaths due to breast cancer up to year 1 (corresponding to between 20 [95% CI 15–25] and 63 [57–70] additional deaths), a 6·8–9·1% increase up to year 3 (169 [159–179] to 228 [218–239] additional deaths), and a 7·9–9·6% increase up to year 5 (281 [266–295] to 344 [329–358] additional deaths).
Source: The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study
For colorectal cancer across scenarios A–C, we estimated an 18·2–20·3% increase in deaths due to cancer up to year 1 (921 [894–970] to 1027 [999–1094] additional deaths), a 16·1–17·6% increase up to year 3 (1301 [1257–1411] to 1414 [1371–1568] additional deaths), and a 15·3–16·6% increase up to year 5 (1445 [1392–1591) to 1563 [1534–1592] additional deaths).
In total, 32,583 patients from England were analyzed. The differences between the estimated cancer death trends are likely due to the life-course of cancer and the associated screening options. In other words, cancer types are detected with a variety of methods. For example, esophageal cancer does not have good screening and relies on patients seeking attention soon after symptoms. On the other hand, primary care physicians conduct a breast exam at most every visit, and mammograms are recommended to most women once reaching a certain age. Regardless, researchers predicted a significant increase in cancer deaths compared to a decade ago. Lastly, this research model assumes the pandemic will last from March 2020 to March 2021. Therefore, a short or longer pandemic period could skew the estimations.
Going forward
“
While residents have taken to social distancing, cancer does not pause. The delay in diagnosis will likely lead to presentation at more advanced stages and poorer clinical outcomes.
JAMA
There is a population of undiagnosed precancerous or cancer cases who are not receiving treatment during the pandemic. Cancer institutes have implemented careful measures to ensure the safety of their current patients as they continue to receive cancer treatment. For the most part, the undiagnosed population is not included in these efforts. A concern for cancer can be triggered by any doctor, particularly a primary care doctor. The pandemic has caused a delay in these services that are considered less urgent. Not to mention, some patients fear entering a medical center during the pandemic. But, as the data suggests, the postponing of cancer screenings will ultimately push back treatment for cancer patients.