coronavirus and diabetes: Unique risks and challenges for people with diabetes during the pandemic
During the coronavirus pandemic, everyone has a laundry list of personal risks and challenges. As scientists learn more about the virus, they've identified specific groups most at risk of severe illness. The most at-risk population, as far as we know, are older adults. However, people of all ages have a higher risk of severe illness if they are immunocompromised or have a relevant chronic condition. Type-1 and type-2 diabetes have been recognized as higher-risk conditions.
People with diabetes are at a higher risk of severe illness
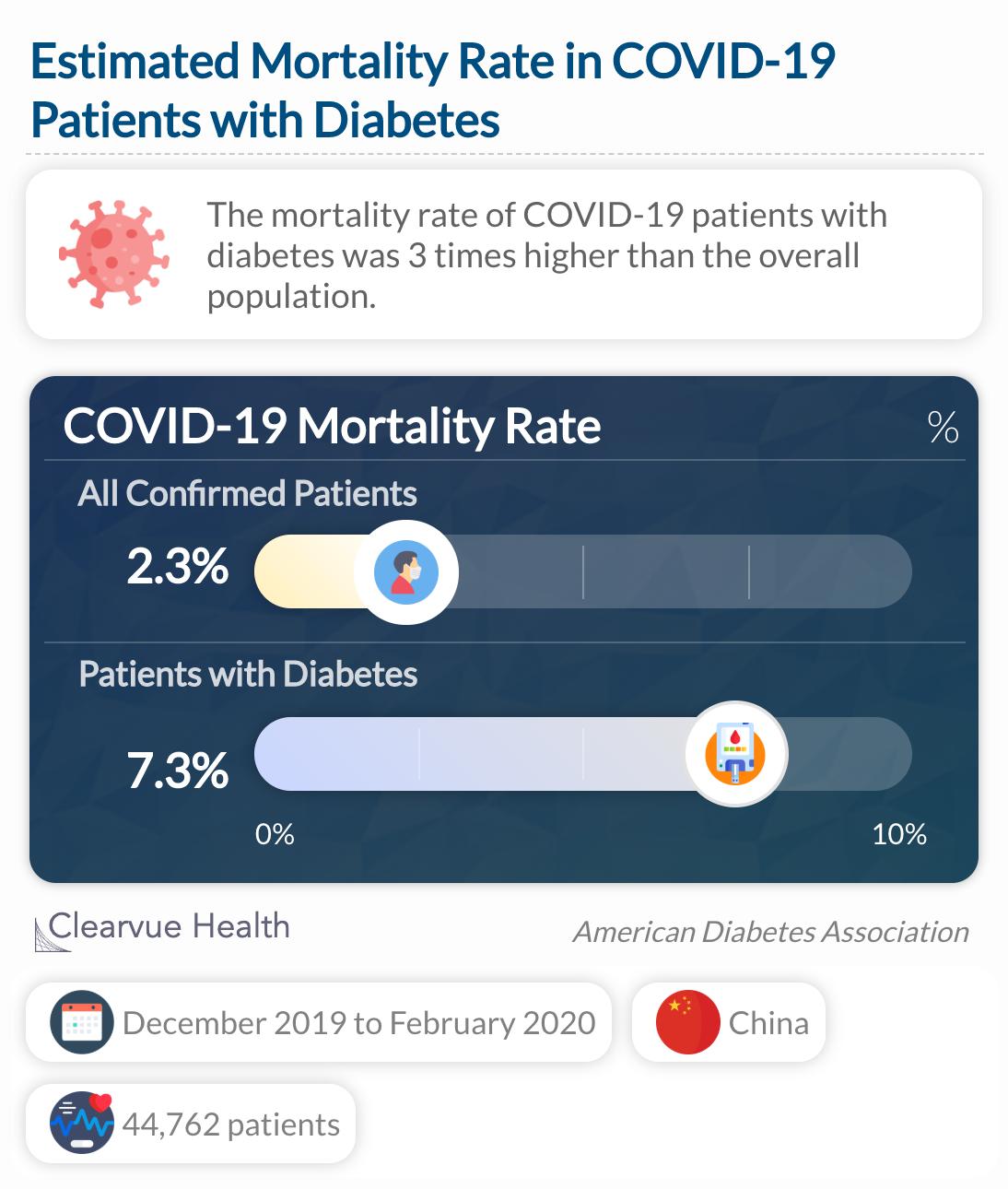
One of the first studies out of China reported the symptoms and demographic characteristics of COVID-19 patients. A total of 44,672 patients diagnosed between December 2019 and February 2020 were included in the report. There are many studies out there that estimate the mortality rate of the virus, but this study is one of the largest. In clinical research, a larger sample is considered more accurate and reduces the likelihood that the findings were due to chance.
Among people with diabetes the mortality rate was 7.3%, more than three times that of the overall population.
Source: COVID-19 in People With Diabetes: Urgently Needed Lessons From Early Reports
Based on this study, the mortality rate of COVID-19 was three times higher among patients with diabetes than the general population. It is important to note that these mortality statistics came from one country at an earlier stage in the pandemic and is not the true, global mortality rate. A mortality rate is actually very difficult to determine. It requires complete surveillance of the virus, including cases with mild or no symptoms. The mortality rate also varies by country, most likely due to the differences in transmission, population health, and available medical care. As of August 2020, scientists estimate the mortality rate to be closer to 1%.
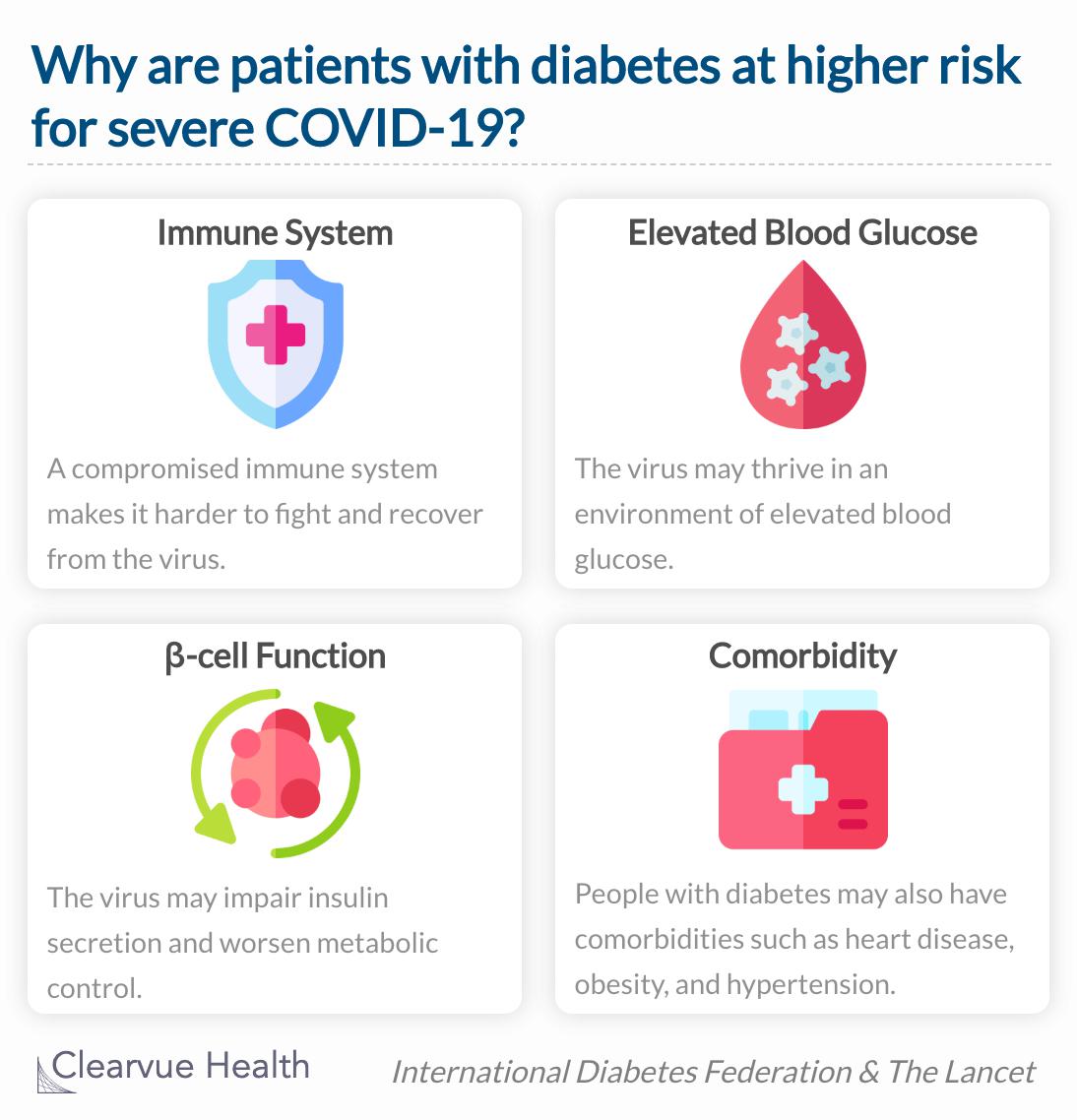
Researchers have a few theories about why people with diabetes are at high risk of severe illness from COVID-19.
The immune system, blood glucose levels, pancreatic cell function, and comorbidities may be mediating the increased risk of serious illness in diabetes infected with the coronavirus.
Source: COVID-19 and diabetes
Source: COVID-19 in people with diabetes: understanding the reasons for worse outcomes
Lost wages or health coverage could lead to medication rationing
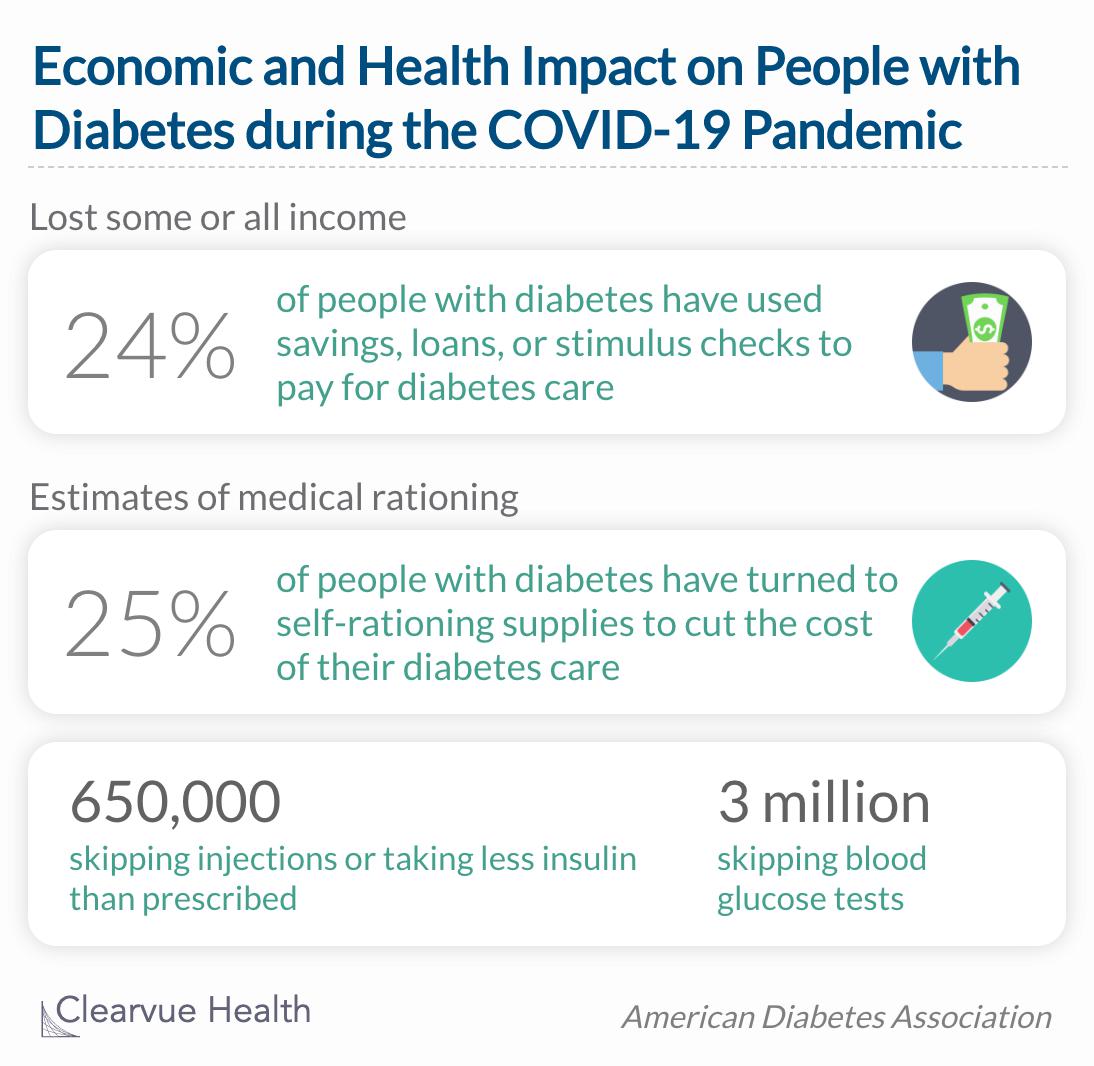
The coronavirus has hurt more than just the people infected. Stay-at-home orders and social distancing rules have disrupted everyone's lifestyles and the strength of the economy. The American Diabetes Association administered a survey to 5,000 people with diabetes nationally to inquire about their health and economic well-being since the start of the global pandemic.
Rationing further increases the likelihood of bad
outcomes from COVID-19 in the short term – and will
drive up the cost of diabetes complications in the
long term.
Source: New Data Highlights Severe Health and Economic Impact of Pandemic on Millions Living with Diabetes
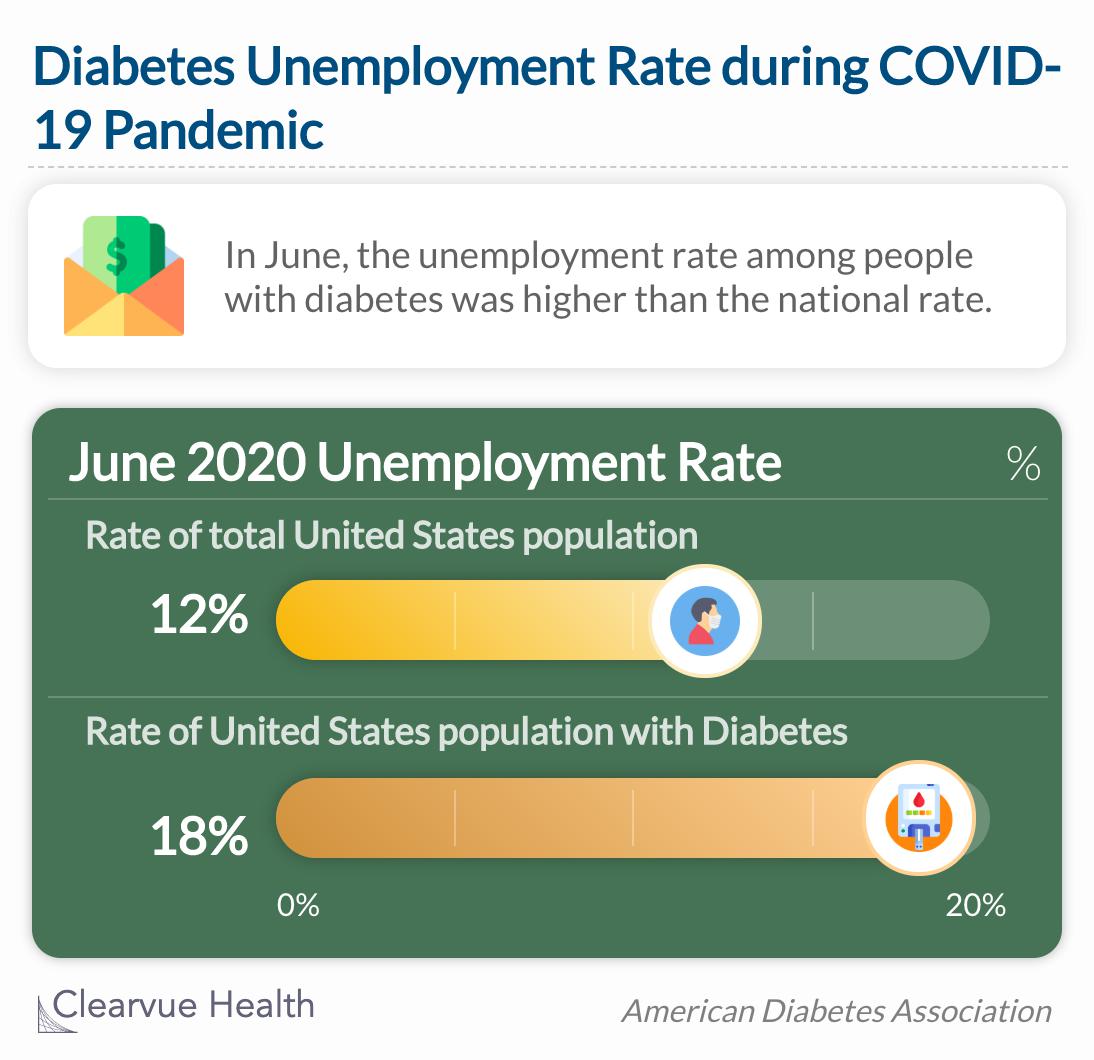
Based on the national survey, researchers estimate that nearly a quarter of people with diabetes have lost some or all of their income since the coronavirus reached the United States. This impact has hit low-income and self-employed people with diabetes the most severely. In addition, they estimate that a quarter of people with diabetes are rationing medication as a result of the pandemic. Rationing medication is not only detrimental to diabetes management but can increase the likelihood of bad outcomes from COVID-19. On top of that, the unemployment rate among people with diabetes was higher than the national rate in June of 2020.
In June, the unemployment rate among people
with diabetes was higher than the national rate at
18% vs. 12%.
Reduced access to insulin and diabetes supplies
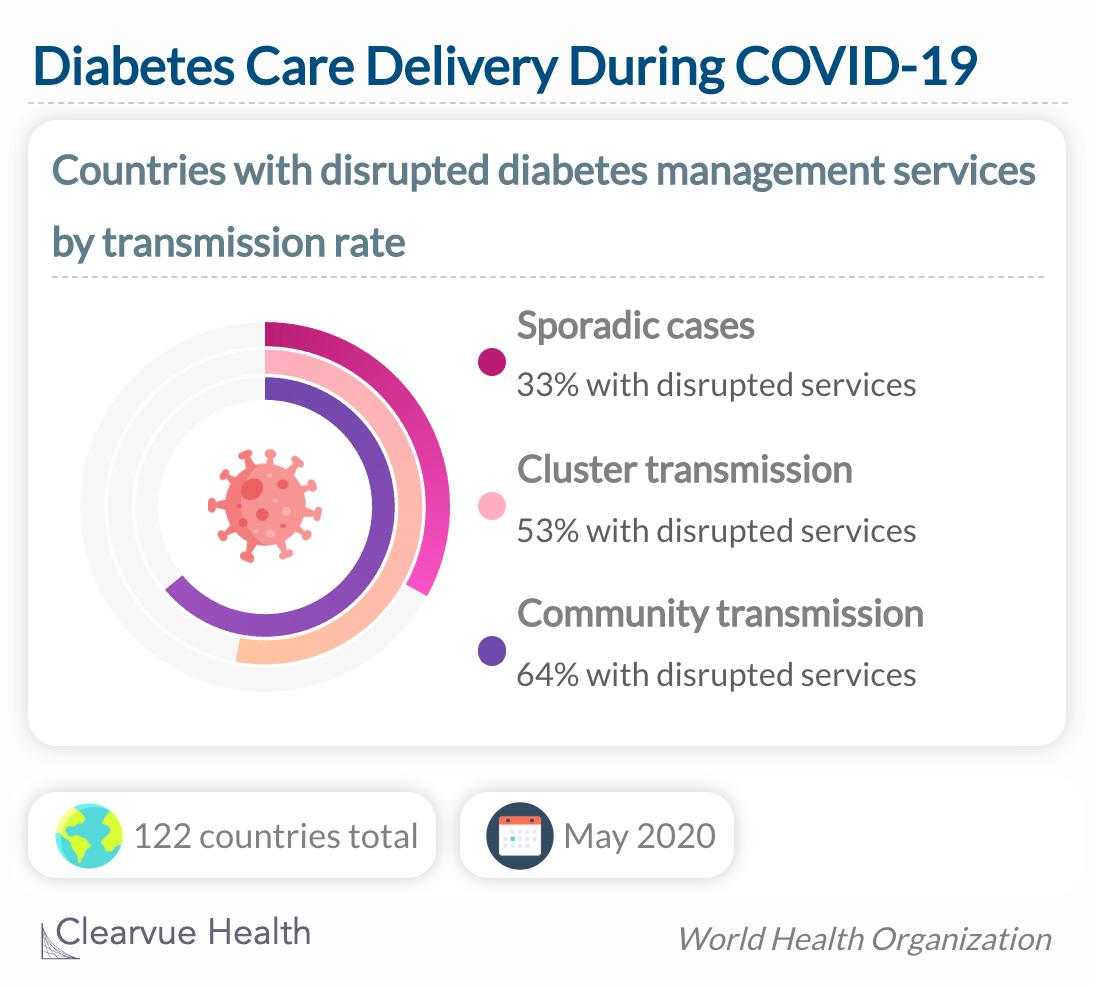
In some countries, restrictions meant to reduce the spread of COVID-19 are actually disrupting the supply chain for insulin and other essential diabetes medicines. The World Health Organization conducted an assessment of service delivery for non-communicable diseases during the pandemic. Researchers categorized countries into three groups: sporadic cases, cluster transmission, and community transmission. These groups describe the magnitude of the countries transmission rate. Countries with sporadic cases reported minimal confirmed COVID-19 cases, while countries with community transmission reported high rates of viral spread.
The World Health Organization (WHO) conducted a rapid assessment of service delivery during the pandemic and found that in the majority of countries surveyed had been disruptions in services to treat diabetes and its complications.
Source: Rapid assessment of service delivery for NCDs during the COVID-19 pandemic
Of the 122 countries examined, 33% of countries with sporadic cases, 53% of countries with cluster transmission, and 64% of countries with community transmission reported disrupted services to treat diabetes and diabetic complications. Examples of service disruption include medical center closures and reduced access to medication. Rehabilitation services, hypertension management, and diabetes management were the top three non-communicable disease services that had been disrupted by the pandemic.
The data tells us that an increase in viral transmissions equates to an increase in diabetes care disruptions. Countries with the most cases and the fastest transmissions are most likely to be unable to provide complete care to patients with diabetes. Even in countries where cases are sporadic, a third of which reported interruptions to their diabetes care delivery systems.
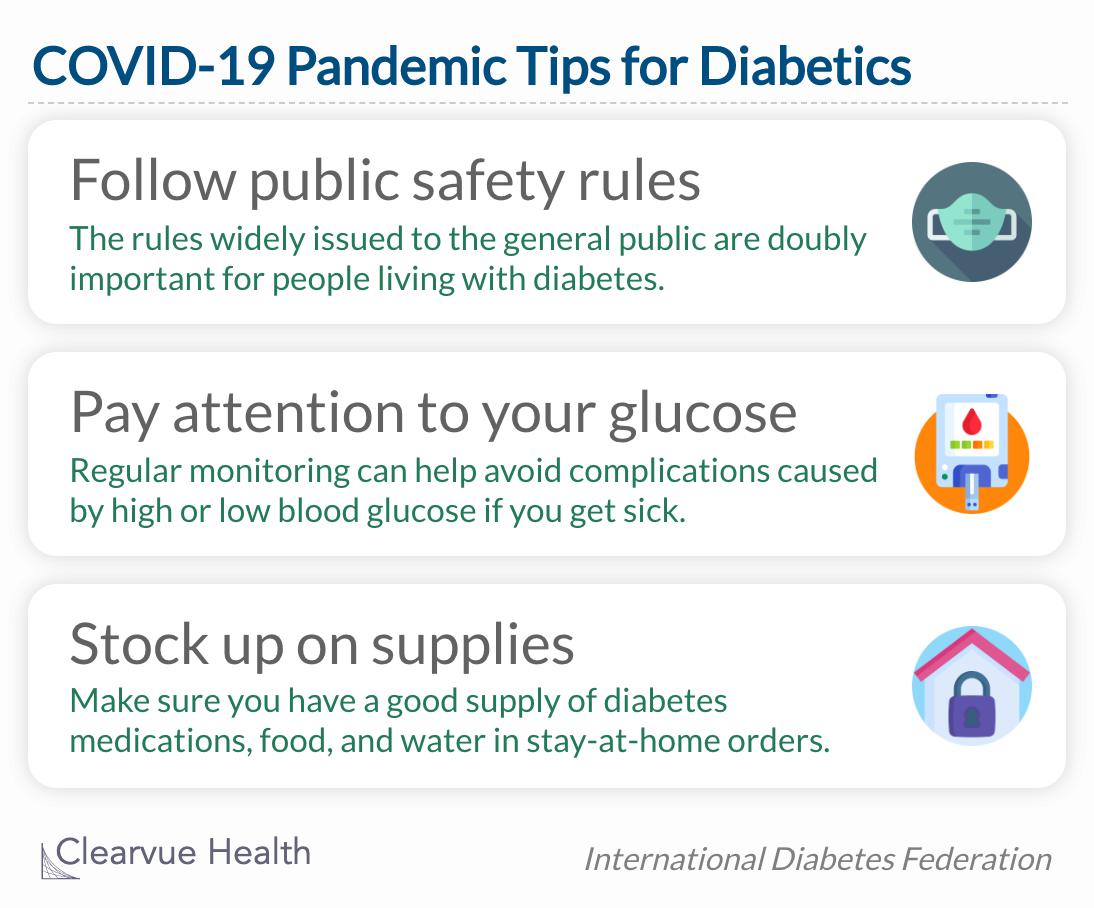
During the pandemic, diabetics are advised to follow all public safety recommendations, pay attention to glucose levels, and stock up on diabetes supplies.